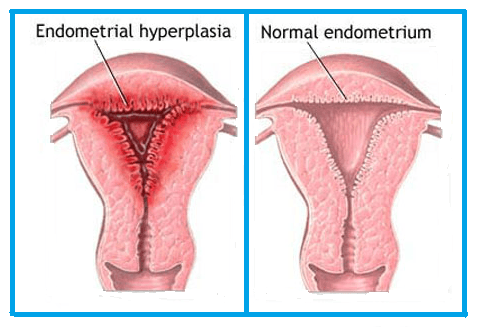
Endometrial Hyperplasia
An uncontrolled growth of endometrial glands is known as endometrial hyperplasia. When the endometrium (uterine lining) thickens excessively, it is known as endometrial hyperplasia. The lining that sheds throughout your menstrual cycle is called endometrium.
Overview
According to estimates, the frequency of endometrial hyperplasia is three times higher than that of endometrial cancer cases. Endometrial hyperplasia may be a sign of endometrial cancer, and if detected early, enough treatment can stop the cancer from progressing. Diagnosing and treating endometrial hyperplasia correctly is necessary to reduce the number of incidences of endometrial cancer. Women in the 50–54 age group are usually diagnosed with hyperplasia without atypia. The age range of 60-64 years is the most common, and under 30 years is the least common age for the condition.
Endometrial hyperplasia is classified into the following types:
Simple or complex endometrial hyperplasia (without atypia): This kind of hyperplasia has cells that appear normal and aren't likely to develop into cancer ("without atypia" indicates less likely to develop into cancer). Your doctor might advise hormone treatment, or the condition might get better on its own.
Atypical endometrial hyperplasia is either simple or complex (with atypia): Endometrial hyperplasia that is “atypical” or “with atypia” is more likely to progress to cancer. Your risk of developing uterine or endometrial cancer rises if you don't get treatment.
Causes
Chronic exposure to estrogen combined with a relative progesterone shortage leads to endometrial hypertrophy. Exogenous or endogenous factors may be the source of high estrogen.
The following are risk factors linked to endometrial hyperplasia:
Genetics: Age, Nulliparity, Obesity, Diabetes mellitus
Cycles of anovulation: PCOS, perimenopause, Granulosa cell tumours, which are ovarian cancers, and hormone replacement therapy. Estrogen-only treatment is not recommended for women who have a uterus since it can cause endometrial hyperplasia at even low doses.
Herbal or over-the-counter remedies could contain a lot of estrogen.
Endometrial hyperplasia may also result from infection or immunosuppression (renal graft recipients).
Women who have Lynch syndrome or hereditary nonpolyposis colorectal cancer are significantly more likely to have endometrial hyperplasia.
Symptoms
Abnormal bleeding during the menstrual cycle or in between periods.
Menstrual periods that are less than 21 days.
Excessive menstrual flow.
Bleeding after menopause.
Amenorrhea, or not getting a period at all.
Many of these symptoms are typical of those going through the menopause. Unpredictable bleeding, irregular periods, or missing periods are common symptoms of entering menopause.
Ayurvedic View
Asrugdara - here, asrug means menstrual blood, and dara means flow. In this disease, the patient has excessive menstrual bleeding; this is endometrial hyperplasia. Due to causes that aggravate pitta dosha, along with anubandha (mix) of all three dosha, results in heavy bleeding, apana vayu (responsible for downward flow) is also involved more. The Ayurveda way of approach is to correct the imbalance by assessing dosha and its anubandha dosha by Ayurvedic internal and external panchakarma treatment, and further prevent related co-morbidities in this condition.
Endometrial Hyperplasia
Treatment for
DISCLAIMER: Listed treatment details are only for information purposes. Treatments and duration may vary depending on numerous factors. Treatments for your condition may not be limited to this list.






















